Symptoms Of Genital Herpes
Primary Genital Herpes Outbreak
For people with symptoms, the first outbreak usually occurs in or around the genital area 2 days to 2 weeks after sexual exposure to the virus. The first signs are a tingling sensation in the affected areas and groups of small red bumps that develop into blisters. Over the next 2 to 3 weeks, more blisters can appear and rupture into painful open sores. The lesions eventually dry out, develop a crust, and heal rapidly without leaving a scar. Blisters in moist areas heal more slowly than those in dry areas. The sores may sometimes itch, but itching decreases as they heal.
About 40% of men and 70% of women develop other symptoms during initial outbreaks of genital herpes, such as flu-like discomfort, headache, muscle aches, and fever. Swollen glands may occur in the groin area or neck. Some women may have difficulty urinating and may, occasionally, require a urinary catheter. Women may also experience vaginal discharge.
Recurrent Genital Herpes Outbreak
In general, recurrences are much milder than the initial outbreak. The virus sheds for a much shorter period of time compared to an initial outbreak of 3 weeks. Women may have only minor itching, and the symptoms may be even milder in men.
The Management Of Post
Shingles, or herpes zoster, may occur at any stage in a person’s life. Herpes zoster is the clinical manifestation of the reactivation of a lifelong latent infection with varicella zoster virus, usually contracted after an episode of chickenpox in early life.1 Varicella zoster virus tends to be reactivated only once in a lifetime, with the incidence of second attacks being < 5%.2 Herpes zoster occurs more commonly in later life and in patients who have T cell immunosuppression.
Pain persisting after herpes zoster, termed post-herpetic neuralgia, is the commonest and most feared complication. Its definition is controversial, ranging from pain persisting after the rash heals to pain persisting 30 days or 6 months after the onset of herpes zoster. Some experts consider all pain during and after herpes zoster as a continuum. Therefore we have suggested that this total duration of pain and pain at a single time point be used as endpoints in clinical studies.3 Post-herpetic neuralgia is associated with scarring of the dorsal root ganglion and atrophy of the dorsal horn on the affected side, which follows the extensive inflammation that occurs during herpes zoster. These and other abnormalities of the peripheral and central nervous system produce the pain and other unpleasant symptoms of post-herpetic neuralgia, which include allodynia , and hyperalgesia.4
No Ulcers Doesnt Equal No Herpes So Then What
If youve never had genital ulcers and as far as you know, have never been exposed, is it worth getting tested? Thats a controversial point and in fact, the widely followed official guidelines discourage screening.
Why? Many reasons: Lets say a person has a blood test that comes back positive for HSV-2. This means that the patient may have been exposed to HSV-2 at some point in their lives, somehow, somewhere. Research tells us that these folks may be periodically shedding virus particles in their genital fluids. These patients would then be diagnosed with genital herpes, encouraged to share their status with future partners, and offered daily antiviral medication to prevent possibly spreading the virus.
All of this can be a tough pill to swallow, so to speak. There is significant social stigma and shame associated with herpes. In addition, there are occasionally false-positive tests. Labeling someone with the diagnosis can be devastating to their future relationships, and asking someone to take a pill for a condition they may or may not have and may or may not spread seems unreasonable.
However, not all experts agree with the official guidelines. Except for the uncommon case of a false positive blood test for HSV-2, a seropositive test means one of three things:
If you are not sure about getting tested, talk with your doctor.
About the Author
Also Check: Can You Sue Someone For Knowingly Giving You Herpes
Diagnosis And Treatment Process
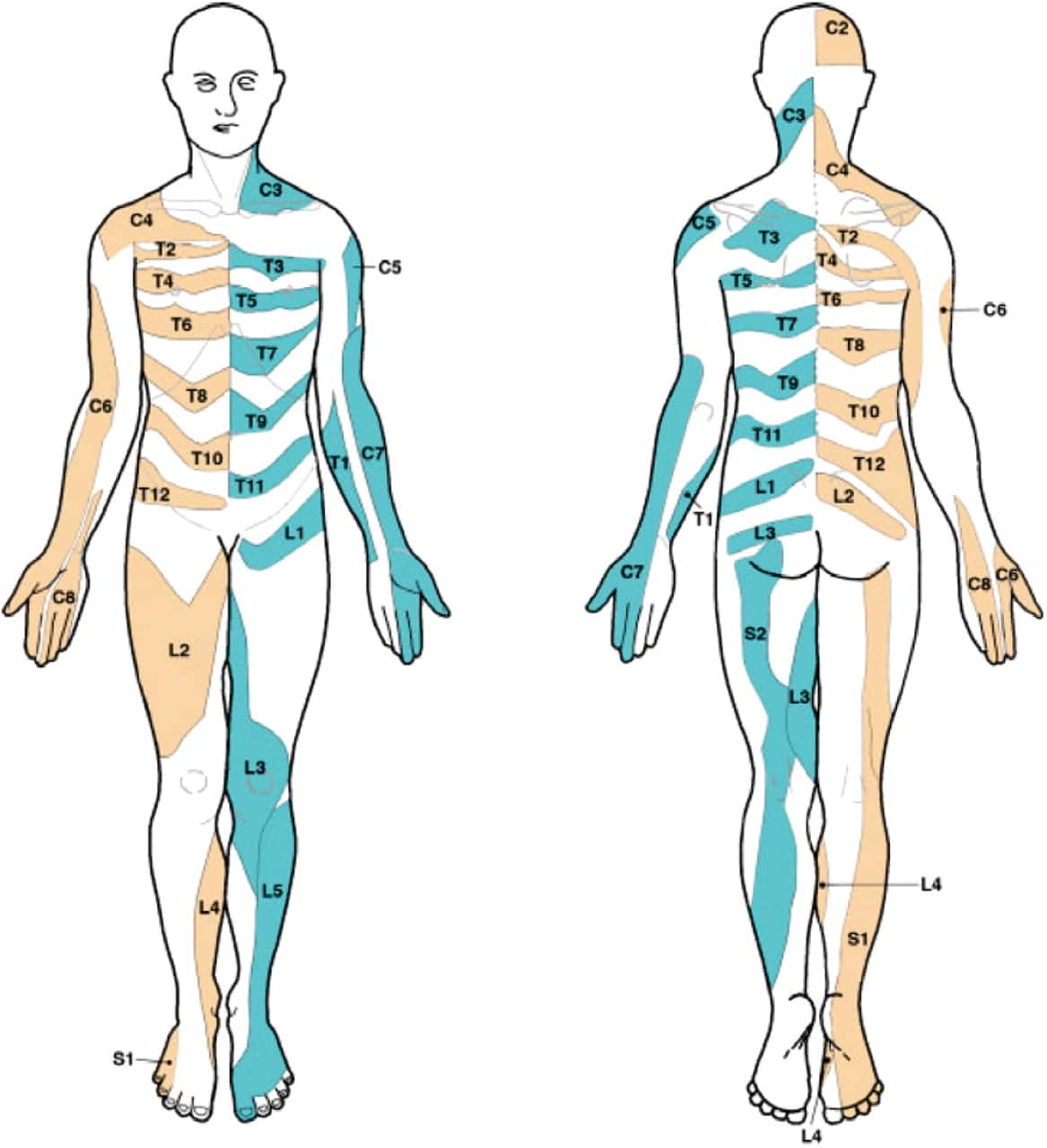
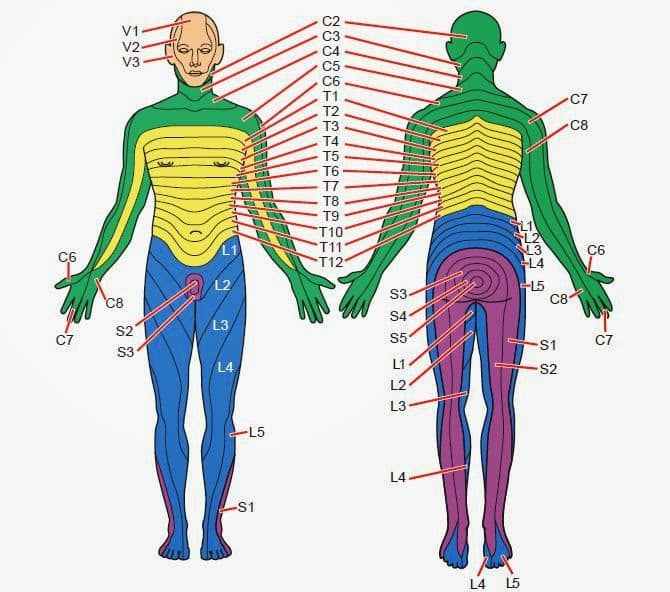
After 3 days of admission, we examined the body for 3 times successively, and herpes-like skin lesions on the right hip and right calf were found gradually, and local skin was of tenderness . After consultation with a dermatologist, the diagnosis was amended as sciatic herpes zoster in the right lower extremity. Oral administration of famciclovir was recommended and then to observe changes of the symptoms. After 3 days of treatment, the pain in the right lower extremity was of obvious relief, and VAS score was down to 2 points. Physical examination showed that the right lower extremity rash is partially scarred , and the extent of inflammation was subsided significantly. After the treatment, the patients were followed up for one and three months: the pain in the right lower extremity was totally relieved, VAS score was 0, and the rash in the right lower extremity was completely subsided.
Figure 4. 3 days after admission, the patient was found to have herpes simplex lesions on the lateral right hip and right calf. The lesion of the right lower extremity was slightly relieved after taking famciclovir for 3 days.
When Does It Happen

Since herpetic nerve pain often occurs before an outbreak, it may be a herpes prodrome symptom. Prodrome symptoms are the warning signs you might sometimes get when you are about to have an outbreak.
The good news is that prodrome symptoms can help someone know to start treatment before a full-blown outbreak occurs.
You May Like: Where To Get Herpes Medication
How Can I Manage The Symptoms
- Keep the area clean to avoid infection. You can use an ice pack wrapped in a towel to reduce pain and soothe your skin.
- Some people find topical anaesthetic creams such as Emla help
- Drink plenty of fluids â this will dilute your urine and make passing urine less painful.
- Avoid tight clothing as it may irritate the blisters and sores further.
Can Herpes Meningoencephalitis Be Prevented
Avoiding herpes virus infections in the first place can help you prevent herpes meningoencephalitis. Ways to avoid infections from herpes viruses include:
-
Abstain from sex or have only one sex partner who has been tested for the virus and isn’t infected.
-
Use a latex condom, which can reduce but not entirely prevent the risk of infection.
-
Avoid kissing people with cold sore blisters. It’s important to keep in mind that most people have already been infected with HSV1 virus by the time they’re 20 years old. If you’ve already been infected, the virus goes dormant inside your body except during outbreaks.
Some pregnant women who have had genital herpes outbreaks may want to have their babies delivered by cesarean section. This may prevent meningoencephalitis in newborns.
Don’t Miss: Getting Rid Of Herpes Scar
Recovery From The Nerve Pain In The Leg
The above-mentioned home remedies and proper medications are essential elements to recover nerve pain in the leg quickly. In addition, a positive mental attitude and back to the job for limited times also prove effective in this recovery process.
Surgical methods take some time to heal correctly. But by following all instructions given by doctors, patients can recover nerve pain completely.
What Are The Causes Of Nerve Pain In The Legs
Some commonly known causes of nerve pain in the legs are described below:
- Diabetes is the leading cause of nerve damage and pain in the legs. Researchers think that with time, high blood sugar levels harm nerves of the whole body, especially in the legs. It leads to interfering negatively with the nerve abilities to transmit signals. Consequently, this outcome results in diabetic neuropathy. Besides this, high blood sugar destroys the walls of the capillaries , which provide nutrients and oxygen to the nerves.
- Human immunodeficiency virus is also one of the leading causes of nerve damage and, ultimately, pain in different body regions. Primarily, this virus affects sensory and motor nerves in the distal parts of the limbs resulting in HIV neuropathy. This virus can affect many nerves simultaneously or affect only one at a time.
It is found that HIV neuropathy has become standard worldwide among HIV patients nowadays. These patients have affected more peripheral nerve disorders. HIV neuropathy is always based on clinical examination, patients history, and advanced supporting laboratory investigations.
Other risk factors that cause nerve pain in legs:
Besides these causes, as mentioned above, certain risk factors induce nerve pain in the legs.
Once nerves become damaged, it automatically induces pain in affected parts of the body. In addition to this pain, compression or inflammation causes numbness, shooting sensation, and electric-like feeling in affected regions.
Don’t Miss: Home Remedies For Genital Herpes Outbreak
What Happens At A Sexual Health Clinic
The doctor or nurse at the sexual health clinic will:
- ask about your symptoms and your sexual partners
- use a small cotton bud to take some fluid from 1 of your blisters or sores for testing
The test cannot:
- be done if you do not have visible blisters or sores
- tell you how long you have had herpes or who you got it from
Symptoms might not appear for weeks or even years after youâre infected with the herpes virus.
Surgical Treatments For Nerve Pain In The Leg
Doctors recommend surgical treatments in the most severe cases. And mostly when non-surgical methods become ineffective. Despite these, doctors also suggest surgery in one of the following cases.
- Cancer or tumors.
- Complete loss of bowel or bladder functions.
- Extreme leg weakness or numbness.
People always primarily visit an average care physician to diagnose and treat nerve pain in the legs. Unfortunately, these primary care physicians can only prescribe some medications or home-based remedies for pain. But in severe cases, they always recommend an excellent specialist to perform some surgical treatments.
Read Also: Home Remedies For Genital Herpes Outbreaks
Unexplained Causes Of Nerve Pain In The Leg
Despite these causes mentioned above and factors, there are still some unexplained causes for the nerve pain in the legs. In addition, there are specific nerve damages at some points about which neurologists know nothing regarding questions like what, when, and why.
About 15 million to 20 million people have nerve pain in their legs, unidentified as doctors dont know about their primary cause. Its likely to affect people with age more than 60 without having any proper and defined reason.
Can Genital Herpes Be Treated
Your physician can prescribe different medications to help reduce your symptoms and speed up the healing of an outbreak. These medicines work best when you start them soon after an outbreak occurs.
To reduce pain during an outbreak:
- Sit in warm water in a portable bath or bathtub for about 20 minutes. Avoid bubble baths.
- Keep your genital area clean and dry, and avoid tight clothes.
- Take over-the-counter medications, such as acetaminophen or ibuprofen. Avoid aspirin.
Let your physician know if you are worried about your genital herpes. He or she can recommend a support group to help you cope with the virus.
Recommended Reading: How Can You Know If You Have Herpes
Asymptomatic Shedding Of Herpes Virus
Intermittent shedding of HSV from genital skin may occur without symptoms or with unrecognised minor symptoms. The frequency of asymptomatic shedding is more common in those with type 2 genital herpes and in those who have been infected recently. Shedding is most likely to occur in the week before or after a recurrence.
The amount shed from active lesions is much greater than between episodes. This is when the infection is most likely to be passed on, and sexual contact should, therefore, be avoided. One study of couples who avoided sexual contact during recurrences found that, over 12 months, only 1 out of 10 passed the virus on to their partner. In that study, condoms were not used. Using condoms may reduce the risk of infection even further.
How Do You Prevent Shingles
Vaccination is a safe and effective way to protect against shingles in most people. The shingles vaccine should not be given to people who are immunocompromised.
For more information on shingles immunisation, see Shingles immunisation service.
Shingles is less contagious than chickenpox. The risk of spreading the disease is low if the rash is covered. When the rash has developed crusts, you are no longer infectious.
If you have shingles, you should:
- wash your hands often to prevent the virus from spreading.
Avoid contact with these people until the rash has developed crusts:
- pregnant women who have never had chickenpox or the chickenpox vaccine
- premature or low birthweight babies
- children who have not had chickenpox or the chickenpox vaccine
- people with weakened immune systems, such as people who:
- have had chemotherapy
- are taking other medicines that weaken their immune system
- have had a transplant
- are living with HIV.
Also Check: Why Does Herpes Flare Up
How Long Does Postherpetic Neuralgia Last
Postherpetic neuralgia can last for weeks, months, or in some people, years after the shingles rash goes away. In most people, shingles pain goes away in one to three months. However, in one in five people, pain lasts more than one year.
The pain from PHN can be so severe in some people that it disrupts their life. Researchers dont know why some people have severe or long-lasting pain and others do not.
How Can I Sleep With Nerve Pain
Some sleeping positions can help you sleep in a better way if you are having nerve pain. These positions include sleeping on one side of the body, having a pillow in between your thighs, sleeping on your back with a pillow under your legs. Sleeping in a recliner is also a recommended position for people having nerve pain in their legs.
Also Check: How To Stop Itching From Herpes Outbreak
How Long Do Symptoms Last
The initial outbreak of herpes symptoms is usually the most severe and can last up to six weeks before going into remission. Recurring outbreaks are typically less severe, and can last anywhere from a few days to about two weeks. Some people experience more severe symptoms than others and not everyone infected with herpes will experience symptoms.
If you are experiencing tingling in your feet and any other herpes symptoms, visit your local FastMed location. We can perform an STD test to determine if you are infected with herpes and if so, can prescribe the necessary medication to treat it.
You May Like: What Medicine Is Used To Treat Herpes
How Are Oral Herpes Simplex Virus Infections Diagnosed
- Fluid sample: A sample is taken from the affected area and checked under the microscope or sent for other testing.
- Blood tests: Your blood is tested for antibodies and to see if you have been exposed to HSV. The tests may also show if you have developed antibodies from exposure to HSV.
- Biopsy: This is a procedure used to remove a small piece of tissue from the ulcer. This sample is then sent to the lab for tests.
Also Check: How To Stop Mouth Herpes Outbreak
Recommended Reading: Can Herpes Cause Cervical Cancer
Ordering Diagnostic Nerve Blocks For Nerve Pain In Legs
Doctors typically call diagnostic nerve blocks to check nerve irritations and nerve compressions. These nerve blocks contain anesthetic solutions that are injected near the affected nerves. If this solution proves helpful in relieving pain, then doctors consider it as a diagnosis of neuropathy.
After a complete diagnosis, the doctor prescribes some medications or treatments. Both surgical and non-surgical treatments are used to cure nerve pain in the legs.
Sciatic Herpes Zoster Suspected Of Lumbar Disc Herniation: An Infrequent Case Report And Literature Review
- 1Department of Orthopeadics, Tangdu Hospital, Fourth Military Medical University, Xi’an, China
- 2School of Basic Medicine, Fourth Military Medical University, Xi’an, China
- 3Tangdu Hospital, Fourth Military Medical University, Xi’an, China
Background: The symptoms of sciatic herpes zoster are sometimes difficult to distinguish from sciatica caused by lumbar disc herniation. We describe a case of suspected lumbar disc herniation with sciatic herpes zoster to reduce the rate of misdiagnosis.
Case Report: A 55-year old man, male, developed low back pain after carrying heavy items 20 years ago. Characteristics of symptoms: 1. Symptoms were aggravated in the upright lumbar forward flexion position 2. The VAS score was 89 points and the VSA score was 0 point 3. It can be relieved when rested in the supine position 4. It came on intermittently with radiation pain in the right lower limb. There were several attacks every year. One month ago, there was radiating pain in the right lower limb. The pain was from the back of the right hip, behind the thigh, in lateral crural region, to the back of the foot. And Symptoms worsened for 10 days. The VAS score was 8 points. Pain could not be relieved by rest or changing posture. There was no back pain, no lower limbs, weak walking, no claudication and other symptoms. Analgesics and neurotrophic drugs are ineffective. After the application of antiviral drugs, the radiation pain in the right lower extremity was significantly relieved.
Don’t Miss: What Medication For Herpes Outbreak
Who Is At Risk Of Getting Postherpetic Neuralgia
Factors that increase the risk of developing postherpetic neuralgia include:
- Older age: The chance of developing postherpetic neuralgia increases with age. If youre older and develop shingles, youre more likely to develop PHN and have longer lasting and more severe pain than a younger person with shingles. About 10 to 13% of people over age 50 who have had shingles will get PHN. People under age 40 rarely get PHN.
- Weakened immune system: Your immune system weakens as you get older, which allows the inactive varicella-zoster virus to become active again and cause shingles in some people. Medical conditions that can weaken your immune system include cancer, chronic infectious diseases , being an organ transplant recipient or taking medications that weaken your immune system .
- Severity of your shingles: If you have a severe rash, you have a greater chance of PHN.
- Painful, itchy or tingly feeling before shingles rash: If you had these symptoms in an area of skin a few days before your shingles rash broke out, you are at higher risk of PHN.
- Waiting to see your healthcare provider after shingles rash: If you wait longer than three days after your rash appeared missing the window to receive antiviral drugs you have an increased chance of PHN.