What Does Recurrent Herpes Look Like
Recurrent herpes occurs in the area where it first appeared, though most of the time, there are fewer blisters or a milder outbreak than the first time. Although the face is the most common site of infection, other areas of the body may be involved:
In recurrent herpes, it often takes 7-10 days before the ulcers completely disappear and the skin returns to normal.
Medical Treatment For Oral Herpes
Oral herpes symptoms may resolve without treatment within one to two weeks.
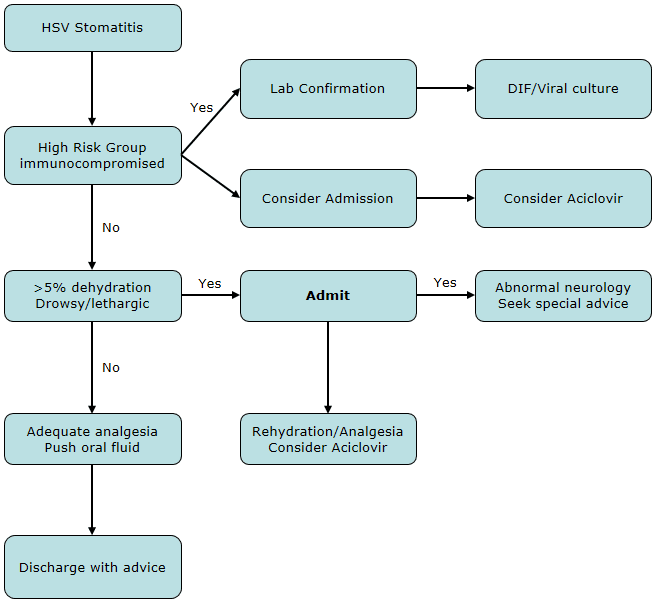
If needed, your healthcare provider will prescribe certain antiviral medications to treat your condition. These medications help with any pain you may be experiencing as well as alleviate symptoms more quickly.
Medications that are used to treat HSV-1 include acyclovir, famciclovir, and valacyclovir, which are most effective if taken when initial warning signs of an incoming flare-up appear and before blisters develop.
Monitoring Of Response To Therapy And Adverse Events
Acyclovir, valacyclovir, and famciclovir are occasionally associated with nausea or headache. No laboratory monitoring is needed for patients receiving episodic or suppressive HSV therapy unless they have advanced renal impairment. However, for patients receiving high-dose IV acyclovir, monitoring of renal function, and dose adjustment as necessary, are recommended at initiation of treatment and once or twice weekly for the duration of treatment.
HSV-2 shedding and GUD can increase in the first 6 months after initiation of ART, particularly in those with low CD4 counts.34,35 Mucocutaneous lesions that are atypical and occasionally recalcitrant to therapy have been reported in individuals initiating ART and have been attributed to immune reconstitution inflammatory syndrome .36
Read Also: Can The Emergency Room Test For Herpes
Genital Herpes Guide: Treatment And Follow
Treatment and follow-up guidance for the genital herpes.
Note: This guide provides minimal information about neonatal herpes. For more information, refer to the Canadian Paediatric Society Position Statement about the prevention and management of neonatal herpes simplex virus infections.
What Is The Prognosis For Oral Herpes Can They Be Cured
Currently, there is no cure or vaccine for herpes simplex virus. Avoiding risk factors, such as sunburn and stress, can help prevent additional outbreaks. Cold sores will usually heal within 2 weeks without treatment. However, there are established cold sore treatments available to help decrease healing time, reduce pain, and in specific cases, suppress the recurrence of the virus.
Cold sores, if they recur, are most likely to do so during the first year after infection. They usually resolve on their own within 1-2 weeks. After the initial outbreak, cold sores may never appear again, or appear only when something triggers them. Usually people with cold sores lead normal lives and are not terribly affected by them unless they happen to recur very often .
Don’t Miss: Herpes Simplex 2 Symptoms Female
Treatment Of Cold Sores
Currently, there are no cures or vaccines for cold sores caused by the herpes simplex virus . Frequent hand washing will help reduce the spread of the virus to other parts of the body or to other people. Also, applying cool, moist compresses to the lesion may decrease pain and keep the lesion from drying and cracking.
- Many people acquire the virus and have no symptoms or signs.
- For others, painful fluid-filled small blisters appear near the area where the virus entered the body.
- Typically, the blisters heal completely but may reappear at some point in the future.
- In between attacks, the virus resides deep in the roots of the nerves of the involved area.
- When herpes simplex flare-ups appear in their most common location, around the mouth, chin, and upper lip, people often refer to them as “cold sores” or “fever blisters.”
- Oral herpes may cause ulcers, fluid-filled blisters, or sores anywhere inside the mouth, including the gums and the tongue.
- It may also cause sores inside the nose and around the nostrils. Herpes may also affect the eye.
What Makes Herpes Recur
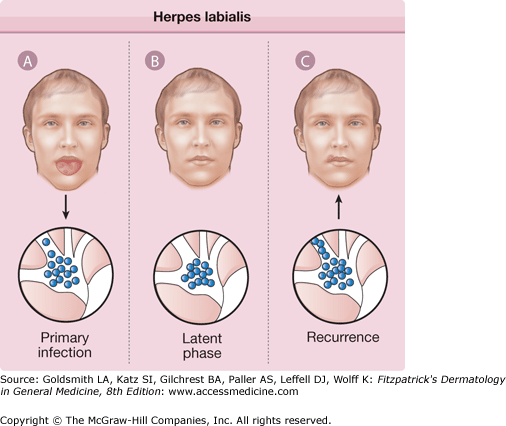
After infection, the virus enters the nerve cells and travels up the nerve until it comes to a place called a ganglion. There, it resides quietly in a stage that is referred to as “dormant” or “latent.” At times, the virus can become active and start replicating again and travel down the nerve to the skin, causing a cold sore outbreak. The exact mechanism behind this is not clear, but it is known that some conditions seem to trigger recurrences, including:
- fever, cold, or the flu
- emotional or physical stress
- weakening of the immune system and
- trauma to the involved area such as dental work.
Sometimes, however, there is no apparent cause of the recurrence.
Also Check: Can Someone With Herpes Donate Blood
What Is Oral Herpes Simplex
Of the herpes viruses, herpes simplex virus type 1 is usually the cause of oral infection. After primary infection, HSV-1 becomes latent, usually in the dorsal root ganglia of the trigeminal nerve. Rarely, herpes simplex virus type 2 may cause primary infection of the oral cavity, typically in association with orogenital sex however, recurrent oral HSV-2 disease is rare.
Treatment Of Primary Infection
Antiviral therapy is recommended for an initial genital herpes outbreak, especially if the patient has systemic symptoms or is immunocompromised.2 Oral acyclovir is effective in reducing symptoms1. Intravenous administration may be required in immunocompromised patients and those with severe disseminated infection.1 Topical acyclovir reduces the duration of viral shedding and the length of time before all lesions become crusted, but this treatment is much less effective than oral or intravenous acyclovir.1
| Symptom/sign |
|---|
Don’t Miss: Herpes Over The Counter Pills
How Do Dermatologists Diagnose Herpes Simplex
During an outbreak, a dermatologist often can diagnose herpes simplex by looking at the sores. To confirm that a patient has herpes simplex, a dermatologist may take a swab from a sore and send this swab to a laboratory.
When sores are not present, other medical tests, such as blood tests, can find the herpes simplex virus.
What You Need To Know
- Fifty percent to 80 percent of U.S. adults have oral herpes.
- Oral herpes can be spread through intimate contact with someone who is infected.
- Oral herpes can be difficult to diagnose. Often confused with many other infections, it can only be confirmed with a virus culture called PCR, blood test or biopsy. PCR is the preferred test for diagnosing herpes infections.
- The best treatment for oral herpes is antiviral oral medication. Symptomatic treatment may include antiviral ointment, over-the-counter topical anesthetics or over-the-counter anti-inflammatory agents.
Whether you call it a cold sore or a fever blister, oral herpes is a common infection of the mouth area that is caused by herpes simplex virus type 1 . Fifty percent to 80 percent of U.S. adults have oral herpes. According to the National Institutes of Health, about 90 percent of adults have been exposed to the virus by age 50.
Once infected, a person will have herpes simplex virus for the rest of his or her life. When inactive, the virus lies dormant in a group of nerve cells. While some people never develop any symptoms from the virus, others will have periodic outbreaks of infections.
You May Like: Can You Donate Blood If You Have Herpes Simplex 2
Episodic Topical Treatment For Recurrent Herpes Labialis
Topical treatment for herpes labialis is less effective than oral treatment. An RCT of treatment with topical penciclovir 1% cream showed healing was marginally faster in the penciclovir group compared with placebo .16 The participants were adults in otherwise good health who had at least three episodes of herpes labialis per year. They applied penciclovir cream or placebo within one hour of the first sign or symptom of a recurrence, and then every two hours while awake for four days. Resolution of symptoms occurred more rapidly in the penciclovir group regardless of whether the medication was applied in the early or late stage. Penciclovir cream applied every two hours while awake reduced median duration of pain from 4.1 to 3.5 days, sped up the healing of classic lesions from 5.5 to 4.8 days, and did not change median time of viral shedding .16
Docosanol cream is a saturated, 22-carbon, aliphatic alcohol with antiviral activity. It is available without prescription. One RCT of 743 patients with herpes labialis showed a faster healing time in patients treated with docosanol 10% cream compared with placebo cream , as well as reduced duration of pain symptoms .17 More than 90 percent of patients in both groups healed completely within 10 days.17 Treatment with docosanol cream, when applied five times per day and within 12 hours of episode onset, is safe and somewhat effective.
What Tests Do Health Care Professionals Use To Diagnose Oral Herpes
Diagnosis of herpes is easily made based on the visual appearance of the lesions, and the best approach is to see a doctor at the first sign of a blister.
If there is concern that the rash may not be herpes, a swab of blister fluid may be collected for viral culture or polymerase chain reaction test. This is most useful in the first 48 hours before the blister has crusted over. If lesions resolve, then cultures are of no help, because there’s nothing left to culture. Culture results take a minimum of 3-5 days.
PCR testing detects herpes DNA, but it is not as readily available as culture and is a very expensive test to do for simple cold sores.
Blood tests for herpes antibodies are not usually needed, since finding antibodies to herpes just means that the body has been exposed to this virus at some point in the past. It does not determine if the current lesion is due to herpes. They can be done, though, if the diagnosis is unclear or there is a specific reason to know for certain.
You May Like: How To Ease Herpes Outbreak
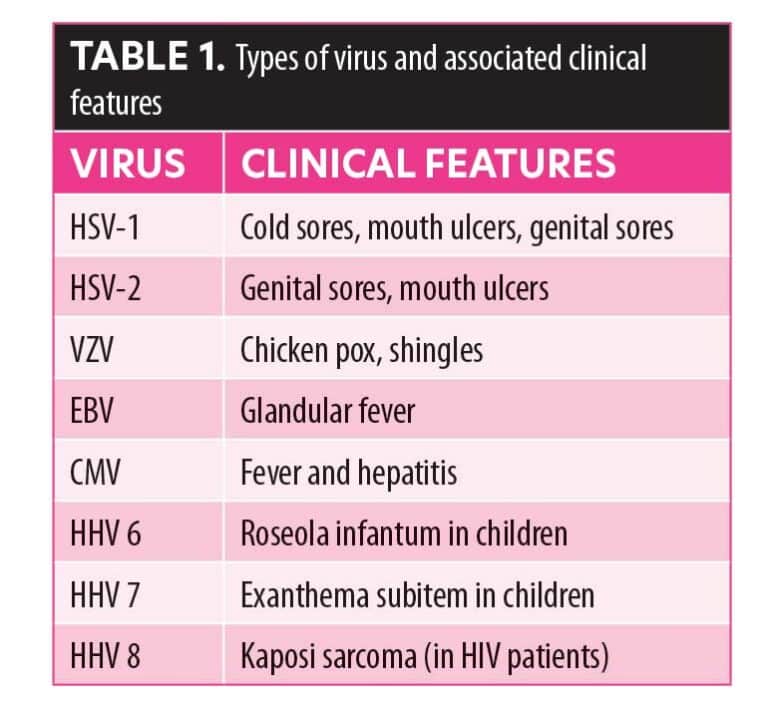
The Virus And Pathogenesis
HSV is a double-stranded DNA virus that may enter the host through abraded skin or intact mucous membranes.1 Epithelial cells are the initial targets. Once infected, these cells die, releasing clear fluid intradermally to form vesicles and merging with other cells to create multinucleated giant cells.
Retrograde transport through adjacent neural tissue to sensory ganglia leads to lifelong latent infection.1 Reactivation of the virus is triggered by local or systemic stimuli such as immunodeficiency, trauma, fever, menstruation, ultraviolet light and sexual intercourse.13 Although emotional stress is assumed to trigger HSV recurrence, recent research fails to show a definite causative role.4 Once reactivated, the virus is transported by the neuron back to the epithelium, where more replication occurs, and another outbreak ensues.
HSV exists as two separate types, labeled 1 and 2, which have affinities for different body sites.2 Ninety percent of infections caused by HSV-2 are genital, and 90 percent of those caused by HSV-1 are oral the reason for this division is unknown.5 In addition, oral HSV-1 infection recurs more frequently than oral HSV-2, and genital HSV-2 recurs more often than genital HSV-1.
Is There A Cure Or Treatment For Herpes
Theres no cure for the herpes virus yet. A herpes vaccine doesnt currently exist, as the herpes virus has more complicated DNA than most infections, creating challenges for researchers.
However, medication can help with symptoms, like sores, and outbreaks. Medication also lowers the risk of transmission to others. You can take most medications for herpes orally, though you may also apply some as a cream or receive them by injection.
Recommended Reading: Does Std Test Include Herpes
Is It Possible To Prevent Cold Sores
The best way to prevent a herpes simplex infection is to avoid physical contact with someone else’s cold sores. Items that touch the lips but cannot be washed or sanitized, such as lipstick or lip balm, should not be shared. During an outbreak, frequent hand washing and sanitizing with 60% ethanol-based hand sanitizer will help reduce the spread of the virus to other parts of the body or to other people. Wash hands immediately after applying topical treatments to a cold sore. L-lysine and other supplements have not been shown to consistently reduce outbreaks.
To prevent future outbreaks:
Special Considerations During Pregnancy
Laboratory testing to diagnose mucocutaneous HSV infections is the same for pregnant women as for non-pregnant women. Episodic therapy for first-episode HSV disease and for recurrences can be offered during pregnancy. Visceral disease following HSV acquisition is more likely to occur during pregnancy and can be fatal. Acyclovir is the antiviral drug with the most reported experience in pregnancy and appears to be safe, particularly during the second and third trimesters .51 One recent caseâcontrol study suggested a higher risk of gastroschisis associated with both genital herpes and acyclovir use during the first trimester of pregnancy.52 The use of valacyclovir and famciclovir during pregnancy has been described, and the antiviral drugs also appear to be safe and well tolerated during the third trimester.53 Given its simplified dosing schedule valacyclovir is an option for treatment and suppressive therapy during pregnancy .
Key: ART = antiretroviral therapy HSV = herpes simplex virus IV = intravenously PO = orally
Also Check: Medicine For Herpes Over The Counter
V Prevention Of Neonatal Herpes
-
Key Question 1: Is there evidence for or against routine screening of pregnant women with HSV type-specific serologies?
The American College of Obstetrics and Gynecology recommends against routine screening for HSV serostatus during pregnancy based on a lack of evidence for cost-effectiveness . It is recommended to screen pregnant women for a history of genital herpes. There are no new data to inform routine screening of pregnant women for serologic evidence of HSV infection.
-
Key Question 2: Should women with HSV-2 infection receive suppressive therapy during pregnancy to reduce the risk of cesarean deliveries, HSV shedding, or HSV transmission to the infant?
Prior randomized clinical trials have demonstrated that women with a history of genital herpes have decreased risk of viral shedding, recurrences, and cesarean deliveries when suppressive acyclovir or valacyclovir 500mg BID is given starting at 36 weeks gestational age . A trial of 200 HSV-2seropositive, HIV-seronegative women in Uganda randomized to receive acyclovir 400mg BID or placebo starting at 28 weeks gestation showed decreased risk of preterm birth and a trend toward decreased risk of premature rupture of membranes at 36 weeks among the acyclovir group . However, additional data are needed to replicate this finding among a larger sample size.
-
Key Question 3: Are there any new data on the safety of HSV antivirals during pregnancy?
Iii Prevention Of Sexual Transmission Of Genital Herpes/management Of Sex Partners
-
Key Question 1: Are there new approaches for prevention of HSV-1/2 transmission from persons with genital herpes infection?
No new data were identified for prevention of HSV-1/2 transmission to sexual partners. The pivotal study performed in HSV-2discordant, HIV-seronegative heterosexual couples showed a 48% decreased risk of transmission for those HSV-2seropositive persons on valacyclovir 500mg daily compared to placebo .
-
Key Question 2: Are there medications that can be taken as preexposure prophylaxis to prevent acquisition of genital herpes?
-
d. There are no data to indicate that antiherpesvirus medication can be taken as PrEP to prevent HSV-2 acquisition.
-
e. What is the impact of taking HIV PrEP on acquisition or reactivation of HSV-2 among HIV-seronegative persons?
Among HIV/HSV-2seronegative men/women in HIV/HSV-2heterosexual discordant partnerships in Africa, daily TDF was associated with 30% reduced risk of HSV-2 seroconversion .
Among MSM and transgender women, daily TDF/FTC was not associated with difference in HSV-2 acquisition, but there was a lower risk of clinically graded moderate to severe ulcers among those randomized to TDF/FTC .
Among MSM, on-demand PrEP was not associated with decreased risk for HSV-2 acquisition .
-
Key Question 3: What is the impact of taking TDF/FTC on acquisition or reactivation of HSV-2 among individuals living with HIV?
You May Like: Can Oral Herpes Be Cured
What Home Remedies And Over
Home remedies
Home remedies include applying a cool wet compress to the lesion to decrease pain and keep the lesion from drying and cracking. Applying compresses too often will cause more drying, however, so a moisturizing balm should be applied after the lesion is first softened with a wet compress. Lemon balm and L-lysine are popularly used as home remedies. While there is there is very limited data suggesting that these substances have antiviral properties, and not enough data to support recommendations, these remedies seem generally well tolerated for those who wish to try them at their own risk.
Natural treatment options provide pain relief and treat cold sores
Lemon balm, L-lysine supplements, citrus bioflavonoids, Lactobacillus acidophilus and bulgaricus, vitamin C, vitamin E oil, and vitamin B12 have also been considered in the potential treatment of herpes simplex virus, but there is no good clinical evidence to support these treatments. Lemon balm may have some anti-herpes properties, but it is impossible to tell if it is effective in affected people from the few laboratory experiments that have been published. L-lysine similarly has limited laboratory data suggesting antiviral properties and has been touted for reducing recurrence of herpes. Unfortunately, results in patients with cold sores have been highly variable and there are no high quality studies suggesting benefit.
What Are The Risk Factors For Herpes Simplex Infections
Exposure to someone with cold sores increases the risk of getting oral herpes. HSV is most contagious when the person has mouth sores or blisters on the lips.
The virus can also be shed from saliva when there are no visible lesions. This is called “asymptomatic shedding.” Therefore, a person can be contagious without having a cold sore outbreak.
- Direct contact with the virus, from kissing or sharing personal items, or skin-to-skin contact, will increase the chance of getting infected with HSV.
- Abnormal areas of skin such as eczema may be especially prone to herpes infection.
- Health care workers, such as dentists, dental hygienists, and respiratory therapists, are at risk of developing herpetic whitlow because of contact with people’s mouths.
- Medical conditions or treatments that weaken a person’s immune system can increase the risk of severe complications from the virus. These include:
Oral herpes is contagious to others who do not have it.
Don’t Miss: Can Herpes Spread In Bath Water