How To Get Rid Of Herpes The Conventional Way
For most people with herpes, the virus typically represents nothing more than an inconvenience however, the real risk is for immuno-compromised patients who cant easily manage infections. In these patients, such as those with HIV/AIDS, herpes simplex infection is associated with increased morbidity and mortality.
As of 2017, there is not currently a herpes vaccine available to prevent HSV-1 or HSV-2.
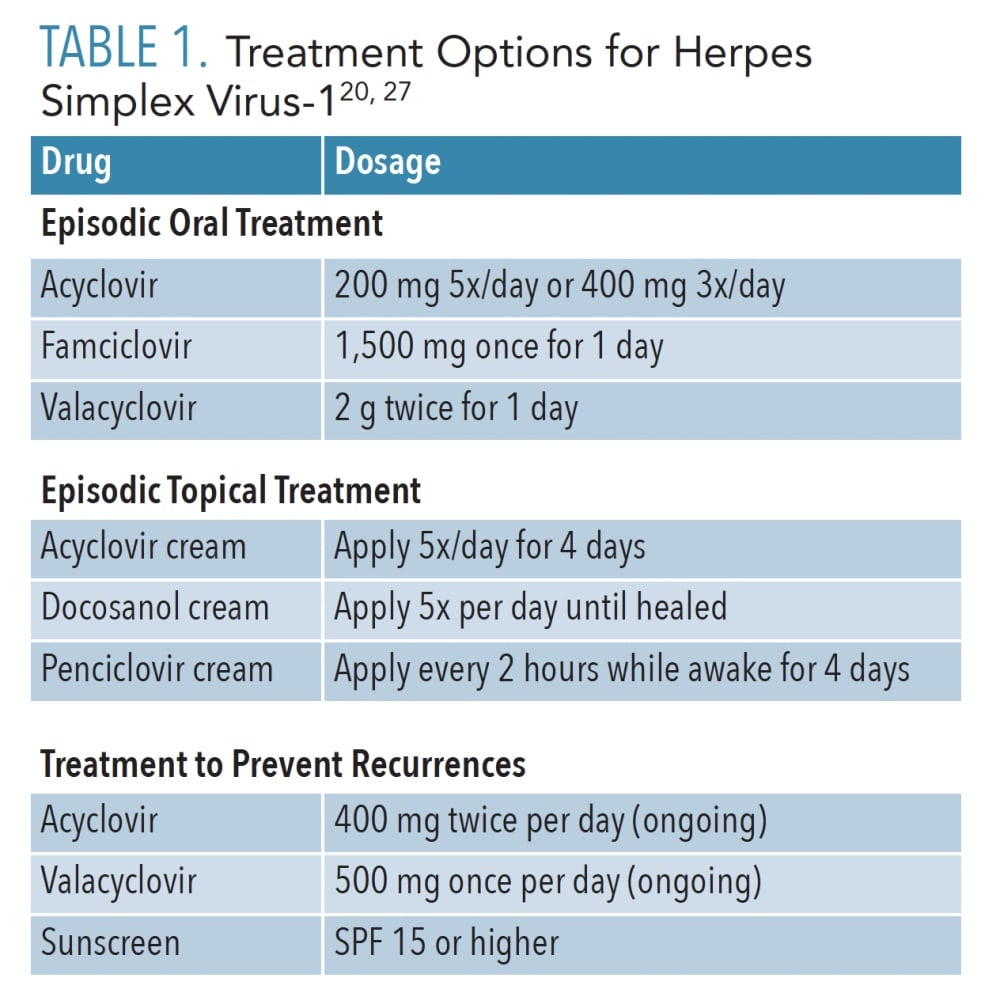
Doctors sometimes prescribe medications to help keep the herpes virus suppressed or to speed up healing of cold sores by reducing bacteria that can cause infections. Some medications that are now used to control herpes include:
- Nucleoside analogues and antiviral medications
- Creams/ointment to help lower pain and inflammation near the site of sores
- Over-the-counter painkillers to reduce aches, tenderness or fever
However, its important to understand that even with early detection and prescription medications, either form of the herpes virus cannot be totally cured so transmission is always still possible. Medications for viruses dont always work long term and are not a cure-all.
Eye Herpes Vs Conjunctivitis
You may mistake eye herpes for conjunctivitis, which is known more commonly as pink eye. Both conditions may be caused by a virus, though conjunctivitis can also be caused by:
A doctor can make the correct diagnosis using a culture sample. If you have eye herpes, the culture will test positive for type 1 HSV . Receiving a correct diagnosis can help you to receive proper treatment.
Monitoring Of Response To Therapy And Adverse Events
Acyclovir, valacyclovir, and famciclovir are occasionally associated with nausea or headache. No laboratory monitoring is needed for patients receiving episodic or suppressive HSV therapy unless they have advanced renal impairment. However, for patients receiving high-dose IV acyclovir, monitoring of renal function, and dose adjustment as necessary, are recommended at initiation of treatment and once or twice weekly for the duration of treatment.
HSV-2 shedding and GUD can increase in the first 6 months after initiation of ART, particularly in those with low CD4 counts.34,35 Mucocutaneous lesions that are atypical and occasionally recalcitrant to therapy have been reported in individuals initiating ART and have been attributed to immune reconstitution inflammatory syndrome .36
Read Also: Dragon Ball Super Super Herp
When To See A Doctor
Because a person might not have symptoms even if they have herpes, it can be difficult to know when to see a doctor for diagnosis and treatment.
Planned Parenthood recommends that a person see a healthcare professional as soon as they notice sores on or around their genitals. Other STIs, such as syphilis, can have similar symptoms but require different treatment. The American Sexual Health Association also recommends seeing a doctor to get a culture of any lesion or cold sore a person notices.
People may wish to take an at-home STI test before seeing a doctor. However, at-home tests should not replace professional diagnosis and treatment.
- applying aloe vera gel to sores
- applying petroleum jelly to the affected areas
- wearing loose clothing to avoid irritation
- refraining from sexual activity, even with protection, until symptoms have gone
- applying a cream or lotion to the urethra before urinating, such as one that contains lidocaine
Some people find that using ice packs help. However, never apply ice directly to the skin wrap it in a cloth first.
Special Considerations With Regard To Starting Antiretroviral Therapy
Orolabial and genital HSV should not influence the decision on when to start ART in persons with HIV. Transient increases in HSV-2âassociated genital ulcers have been observed during the first 6 months after initiation of ART in HIV/HSV-2 coinfected persons. In such cases, suppressive anti-HSV therapy can be considered. The frequency and severity of clinical episodes of genital herpes is often reduced in individuals after immune reconstitution on ART. However, immune reconstitution does not reduce the frequency of genital HSV shedding.33
Read Also: Is Turmeric Good For Herpes
How Does Herpes Simplex Spread
Herpes spreads through close contact with a person who has the infection. The virus can be found in skin and saliva. If you have herpes simplex, you are most likely to pass the virus to another person when you have sores. But you can infect someone else even if you have no symptoms. Healthcare providers call this asymptomatic viral shedding.
People may get HSV-1 through
- Touching a persons skin near the mouth.
- Sharing food utensils, lip balm or razors.
- If you receive oral sex from someone who has a cold sore, it may spread a herpes infection to your genitals.
People may get HSV-2 through
- Oral sex with someone whos infected.
- Touching open sores, including while breastfeeding.
- Childbirth by a mother or gestational parent who has an active infection.
You cant get genital herpes from objects like toilet seats. But you could pass genital herpes through shared sex toys.
Can Herpes Simplex Be Prevented
As sun exposure often triggers facial herpes simplex, sun protection using high protection factor sunscreens and other measures are important.
Antiviral drugs will stop HSV multiplying once it reaches the skin or mucous membranes but cannot eradicate the virus from its resting stage within the nerve cells. They can, therefore, shorten and prevent attacks but a single course cannot prevent future attacks. Repeated courses may be prescribed, or the medication may be taken continuously to prevent frequent attacks.
Read Also: How To Naturally Treat Herpes
Who Is At Risk For Developing Herpes Simplex Infections
Anyone can contract HSV, regardless of age. If youre exposed to HSV, youre likely to contract the virus.
Remember, HSV is very common. But because its often asymptomatic, plenty of people living with the virus never have an episode or realize theyve contracted HSV.
You may have a higher chance of contracting the virus if you:
- have a sexual partner who lives with HSV
- were assigned female at birth . suggests more AFAB folks than people assigned male at birth develop HSV, but this could also mean AFAB folks are more likely to experience symptoms.
- are immunocompromised
Some older research suggests HSV-1 antibodies may offer AFAB folks some protection against contracting HSV-2. Still, many people living with one type of the virus do contract the other type later on. You wont contract the same type of the virus again, though, since it remains dormant in your body once you acquire it.
You may have a slightly higher chance of contracting genital HSV if you have sex without using condoms or other barrier methods. Keep in mind, though, that condoms and other barrier methods wont always cover the infection site, since sores can appear on the buttocks or inner thighs.
Is There A Cure For Herpes Simplex
There is no cure for herpes simplex. Once you have the virus, its a lifelong infection.
What is the outlook for people with herpes simplex?
For many people, the first herpes outbreak is the most severe. Many outbreaks are less frequent and milder after the first year of infection. Some people may have only one outbreak and never have another again.
Herpes infection doesnt usually pose a serious health risk. The risk of a health complication due to herpes is higher in infants and if you have HIV/AIDS, cancer or an organ transplant.
Recommended Reading: Medical Ozone Therapy For Herpes
Suppressive Therapy For Recurrent Hsv
Suppressive therapy reduces frequency of genital herpes recurrences by 70%80% among patients who have frequent recurrences . Persons receiving such therapy often report having experienced no symptomatic outbreaks. Suppressive therapy also is effective for patients with less frequent recurrences. Long-term safety and efficacy have been documented among patients receiving daily acyclovir, valacyclovir, and famciclovir . Quality of life is improved for many patients with frequent recurrences who receive suppressive therapy rather than episodic treatment . Providers should discuss with patients on an annual basis whether they want to continue suppressive therapy because frequency of genital HSV-2 recurrence diminishes over time for many persons. However, neither treatment discontinuation nor laboratory monitoring is necessary because adverse events and development of HSV antiviral resistance related to long-term antiviral use are uncommon.
Valacyclovir 500 mg orally 2 times/day for 3 daysOR
Valacyclovir 1 gm orally once daily for 5 days
*Acyclovir 400 mg orally 3 times/day is also effective, but are not recommended because of frequency of dosing.
Antiviral Creams And Tablets
Antiviral creams such as aciclovir or penciclovir may speed up the healing time of a recurrent cold sore infection if used correctly.
Cold sore creams are widely available over the counter from pharmacies without a prescription.
They’re only effective if you apply them as soon as the first signs of a cold sore appear, when the herpes simplex virus is spreading and replicating. Using an antiviral cream after this initial period is unlikely to have much effect.
If you have frequently recurring bouts of cold sores, use antiviral medication as soon as you feel the tingling sensation that indicates a cold sore is about to develop. You’ll need to apply the cream up to five times a day for four to five days.
Antiviral creams can only help to heal a current outbreak of cold sores. They don’t get rid of the herpes simplex virus or prevent future outbreaks of cold sores occurring.
Antiviral tablets are generally more effective than creams at treating cold sores, but are usually only prescribed for more severe cases.
You May Like: Can You Get Rid Of Herpes Forever
The Virus And Pathogenesis
HSV is a double-stranded DNA virus that may enter the host through abraded skin or intact mucous membranes.1 Epithelial cells are the initial targets. Once infected, these cells die, releasing clear fluid intradermally to form vesicles and merging with other cells to create multinucleated giant cells.
Retrograde transport through adjacent neural tissue to sensory ganglia leads to lifelong latent infection.1 Reactivation of the virus is triggered by local or systemic stimuli such as immunodeficiency, trauma, fever, menstruation, ultraviolet light and sexual intercourse.13 Although emotional stress is assumed to trigger HSV recurrence, recent research fails to show a definite causative role.4 Once reactivated, the virus is transported by the neuron back to the epithelium, where more replication occurs, and another outbreak ensues.
HSV exists as two separate types, labeled 1 and 2, which have affinities for different body sites.2 Ninety percent of infections caused by HSV-2 are genital, and 90 percent of those caused by HSV-1 are oral the reason for this division is unknown.5 In addition, oral HSV-1 infection recurs more frequently than oral HSV-2, and genital HSV-2 recurs more often than genital HSV-1.
Genital Herpes Treatment In Pregnancy

You may be offered antiviral treatment:
- to treat outbreaks in pregnancy
- from 36 weeks to reduce the chance of an outbreak during birth
- from diagnosis until the birth if you first get herpes after 28 weeks of pregnancy
Many women with genital herpes have a vaginal delivery. You may be offered a caesarean, depending on your circumstances.
Recommended Reading: Herpes How Often Do Outbreaks Occur
Understanding Herpes With H Hunter Handsfield Md
Herpes expert H. Hunter Handsfield, MD, explains the basics about genital herpes, including the difference between genital HSV-1 and HSV-2 infection, testing options and the importance of knowing virus type, and the three-prong strategy for prevention. See more herpes videos at sexualhealthTV.com.
Have a question about herpes youd like Dr. Handsfield or our other experts to answer? Visit our Ask the Experts page to learn how.
Who Gets Herpes Simplex
Primary attacks of Type 1 HSV infections occur mainly in infants and young children. In crowded, underdeveloped areas of the world, nearly all children have been infected by the age of 5. In less crowded places, the incidence is lower for example, less than half of university entrants in Britain have been infected. Type 2 HSV infections occur mainly after puberty and are often transmitted sexually.
HSV is transmitted by direct or indirect contact with someone with active herpes simplex, which is infectious for 712 days. Asymptomatic shedding of the virus in saliva or genital secretions can also lead to transmission of HSV, but this is infrequent, as the amount shed from inactive lesions is 100 to 1000 times less than when it is active. The incubation period is 212 days.
Minor injury helps inoculate HSV into the skin. For example:
- A thumb sucker may transmit the virus from their mouth to their thumb.
- A health-care worker may develop herpetic whitlow
- A rugby player may get a cluster of blisters on one cheek .
You May Like: How To Take Valacyclovir For Herpes
How Long Do Sores From Herpes Simplex Last
If youre infected with HSV-1, commonly known as oral herpes, you may notice tingling or burning around your mouth in the days before a cold sore appears. These blisters break open and ooze fluid before forming a crust. Usually, sores last for seven to 10 days.
If youre infected with HSV-2, commonly known as genital herpes, your first outbreak may last between two to four weeks. Recurrent outbreaks usually last between three to seven days.
What Are The Symptoms Of Herpes Simplex
Many people with the infection never experience any herpes symptoms. If you do notice symptoms, youll experience them differently depending on whether youre having your first herpes outbreak or a repeat outbreak. Recurring symptoms are usually milder than the first outbreak. Symptoms dont last as long with later outbreaks. Some people may only have one or two outbreaks during their lifetime. Others may have as many as four or five outbreaks a year.
People who do have herpes symptoms may experience:
- Cold sores around their lips, mouth or tongue. They may look crusty or like fluid-filled blisters.
- Tingling, itching or burning.
- Pain while urinating.
Read Also: Foods To Avoid With Herpes Outbreak
Treatment For Genital Herpes
There are three antiviral medications that are FDA-approved for the treatment of genital herpes:
- Acyclovir: The oldest antiviral medication for herpes is acyclovir. It has been available since 1982 in a topical form and sold since 1985 in pill form. Acyclovir has been shown to be safe in persons who have used it continuously for as long as 10 years.
- Valacyclovir: A newer drug, valacyclovir, actually uses acyclovir as its active ingredient. This medication delivers acyclovir more efficiently so that the body absorbs much of the drug, which has the advantage of taking the medication fewer times during the day.
- Famciclovir: Famciclovir uses penciclovir as its active ingredient to stop HSV from replicating. Like valacyclovir, it is well absorbed, persists for a longer time in the body, and can be taken less frequently than acyclovir.
Antiviral medication is commonly prescribed for patients having a first episode of genital herpes, but they can be used for recurrent episodes as well. There are two kinds of treatment regimens: episodic therapy and suppressive therapy.
Management Of Sex Partners
The sex partners of persons who have symptomatic genital herpes can benefit from evaluation and counseling. Symptomatic sex partners should be evaluated and treated in the same manner as patients who have symptomatic genital herpes. Asymptomatic sex partners of patients who have symptomatic genital herpes should be asked about a history of genital symptoms and offered type-specific serologic testing for HSV-2. For partners without genital herpes, no data are available on which to base a recommendation for PEP or PrEP with antiviral medications or that they would prevent acquisition, and this should not be offered to patients as a prevention strategy.
Don’t Miss: Prescription Cream For Genital Herpes
Home Remedies And Lifestyle
At-home treatments for herpes are used to relieve pain. They do nothing to alter the course of the infection but can make you more comfortable as the herpes sores begin to heal.
There are several things you can do if have an outbreak of oral or genital herpes:
- Use a cold compress. Place a cloth-covered ice pack on the sores for 15 minutes several times daily to reduce pain. Keep the ice pack moving to prevent frostbite.
- Do not touch or scratch. Avoid touching and rubbing the sores. Doing so can spread the infection to other areas of the skin.
- Keep the sores clean. Herpes sores can become infected with bacteria if touched with soiled hands. Wash your hands thoroughly with soap and water after going to the bathroom or before applying medications.
- Reduce stress. Stress can increase your sensitivity to pain during a herpes outbreak. You can reduce stress by performing gentle exercises or practicing mind-body therapies like meditation, yoga, and guided imagery.
To reduce the risk of spreading herpes, avoid kissing and sharing objects that come into contact with saliva, like drinking straws and eating utensils.
Its important to note that oral herpes can be spread to the genitals, and that genital herpes can be spread to the mouth. To reduce the risk of infection, use condoms and dental dams during oral sex. Better yet, avoid sex altogether if you are having an active herpes outbreak .
One Option For Ongoing Therapy: Taking Drugs Regularly
Some people with genital herpes choose to take antiviral medication daily to reduce the number of symptom outbreaks they have. In some cases, daily therapy prevents outbreaks completely.
Numerous studies over the years have demonstrated the safety and effectiveness of all three of the approved antivirals used to treat genital herpes.
Studies have also shown that daily antiviral therapy reduces the rate of transmission from an HSV-2 infected person to an uninfected partner of the opposite sex.
Daily therapy also lowers the odds of infecting other people if you have multiple sex partners or if you are a man who has sex with men.
The drugs work both for people who have had herpes symptoms and for those whose blood tests show they have an HSV-2 infection but who have never had symptoms.
Some people choose to take antiviral drugs only as needed, for outbreaks that occur after the first one. For this to work, you need to start taking the medicine within one day of sores cropping up or during the time period that comes before some outbreaks.
During the prodrome, you may feel
- Burning in the area where the virus first entered your body
- Itching or tingling in that area
- Pain in your back, buttocks, thighs, or knees
Your doctor will probably give you a prescription you can fill and keep handy for timely use, and tell you to start taking the drugs just as soon as symptoms begin.
Read Also: How To Stop Burning When Peeing With Herpes